🚨 Type 5 Diabetes Introduction: A New Chapter in Diabetes Awareness
In April 2025, the International Diabetes Federation (IDF) officially recognized Type 5 Diabetes, also known as Malnutrition-Related Diabetes Mellitus (MRDM) or Severe Insulin-Deficient Diabetes (SIDD). This recognition marks a historic turning point in global health, particularly for developing countries like Pakistan and India, where millions of undernourished individuals have long lived with undiagnosed or misclassified diabetes.
📚 History and Evolution of Type 5 Diabetes
- 1955: First reported case in Jamaica, involving diabetes linked to chronic malnutrition.
- 1985: WHO introduces the term MRDM (Malnutrition-Related Diabetes Mellitus).
- 1999: WHO withdraws the classification due to insufficient global evidence.
- 2005: Dr. Hawkins (USA) advocates for renewed research.
- 2022: A groundbreaking study by the Albert Einstein College of Medicine confirms the presence of unique metabolic characteristics.
- April 2025: IDF officially recognizes this condition as Type 5 Diabetes at a conference in Bangkok, Thailand.
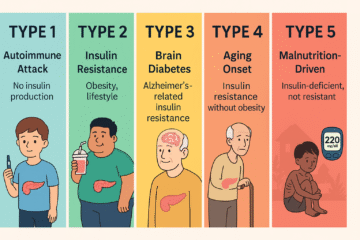
🧬 What Makes Type 5 Diabetes Unique?
In contrast to Type 1 (characterized by autoimmune insulin deficiency) and Type 2 (marked by insulin resistance), Type 5 Diabetes is:
- Caused by protein-energy malnutrition, especially in childhood.
- Found in underweight individuals (BMI < 18.5), often in resource-poor settings.
- Characterized by severe insulin deficiency, not resistance.
- Largely non-ketotic, unlike Type 1.
🧪 How is It Diagnosed?
A series of tests can assist in diagnosing Type 5 Diabetes.:
- C-Peptide Test: Low levels indicate insulin deficiency.
- Autoantibody Panel: Negative for Type 1 markers (GAD, islet cell, insulin antibodies).
- HOMA-IR Test: Indicates no insulin resistance (differentiates from Type 2).
🌍 Global Impact and Importance
- Estimated 20–25 million people globally affected.
- Prevalent in South Asia and Sub-Saharan Africa.
- Comparable burden to diseases like TB and HIV/AIDS in some regions.
- Identifying conditions accurately contributes to improved diagnosis, more effective treatment, and efficient allocation of resources
🍽️ Malnutrition: The Hidden Root of Diabetes
Malnutrition, especially protein-energy malnutrition (PEM), plays a critical role in the development of Type 5 Diabetes.
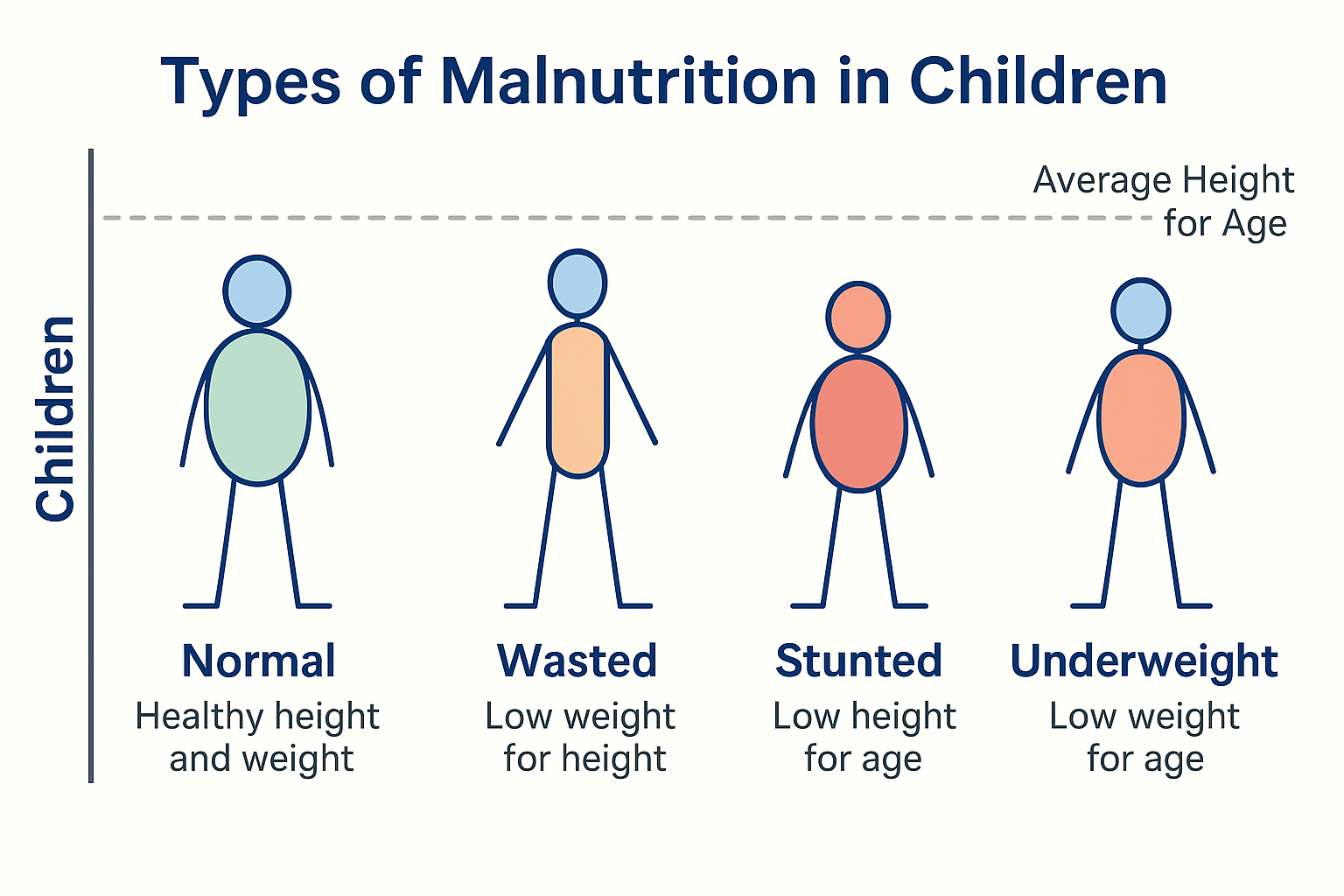
🔹 Forms of Childhood Malnutrition:
- Normal: Healthy height and weight for age.
- Wasted: Low weight for height — acute undernutrition.
- Stunted: Low height for age — chronic undernutrition.
- Underweight: Low weight for age — can be chronic or acute.
These conditions affect pancreatic development and long-term insulin production. Poor maternal nutrition during pregnancy can also impair fetal organ growth, leading to higher diabetes risk later in life.
💊 Treatment Implications
- Unlike Type 1, many patients do not require insulin and may respond to oral medications.
- Emphasis on nutritional rehabilitation, especially protein intake.
- Individualized management depending on severity and coexisting conditions.
✅ Final Thoughts: Why This Matters
- Recognition of Type 5 is a milestone for equity in healthcare.
- It corrects decades of misclassification and mistreatment.
- It emphasizes nutrition as prevention — not just treatment.
- For countries like Pakistan, it’s a wake-up call to address early childhood malnutrition as a driver of metabolic disease.
🔍 Scientific References
- International Diabetes Federation. (2025). New Type 5 Diabetes Working Group Launched. https://idf.org/news/new-type-5-diabetes-working-group
- Tripathy BB, et al. (1983). Malnutrition-Related Diabetes Mellitus. Diabetes Care, 6(5):515–518. https://doi.org/10.2337/diacare.6.5.515
- Wu G, et al. (2016). Protein nutrition and malnutrition in childhood. Advances in Nutrition, 7(2): 234–241. https://doi.org/10.3945/an.115.011254
- Hales CN, Barker DJP. (2001). The thrifty phenotype hypothesis. British Medical Bulletin, 60(1):5–20. https://doi.org/10.1093/bmb/60.1.5
- Boutry-Regard C, et al. (2006). Low-protein diet during gestation and lactation alters the glucose–insulin axis in offspring. Journal of Nutrition, 136(5):1252–1256. https://doi.org/10.1093/jn/136.5.1252
🌿 Let’s not forget: the fight against diabetes must begin with food, especially in the early years of life.